by Haley McRaven
Diabetic foot ulcers (DFUs) represent a significant healthcare challenge in Pasco County, Florida, contributing to morbidity, mortality, and substantial healthcare costs. Conventional treatments often face limitations in promoting timely and effective wound healing. Red light therapy (RLT), a non-invasive therapeutic modality utilizing specific wavelengths of light, has emerged as a promising adjunctive treatment for various conditions, including wound healing. This paper explores the potential benefits of RLT in accelerating the healing of diabetic wounds, examining the underlying mechanisms of action, reviewing existing clinical evidence, and discussing the implications for individuals with diabetes in Pasco County. Factors relevant to the local context, such as the prevalence of diabetes and access to healthcare, will also be considered. While research directly focusing on Pasco County is limited, the synthesis of broader scientific literature suggests that RLT holds considerable promise as a safe and effective tool to improve wound healing outcomes and enhance the quality of life for diabetic patients in this region.
Keywords: Red light therapy, photobiomodulation, diabetic foot ulcers, wound healing, Pasco County, Florida, diabetes mellitus.
Introduction
Diabetes mellitus, a chronic metabolic disorder characterized by hyperglycemia, poses a significant public health burden globally and within the state of Florida, including Pasco County. According to the Centers for Disease Control and Prevention (CDC), a substantial percentage of adults in Florida are diagnosed with diabetes, and this prevalence is projected to rise (CDC, n.d.). A serious complication of diabetes is the development of diabetic foot ulcers (DFUs), which are open sores or wounds that occur in approximately 15% of individuals with diabetes (Armstrong et al., 2017). In Pasco County, with its aging population and increasing rates of diabetes, the incidence of DFUs likely presents a considerable clinical and economic challenge, leading to prolonged hospitalizations, increased risk of infection and amputation, and diminished quality of life for affected individuals (Florida Department of Health, 2024).
Conventional treatments for DFUs typically involve wound debridement, infection control, offloading pressure, and advanced wound dressings (Lipsky et al., 2016). However, these approaches can be time-consuming, costly, and may not always result in complete wound closure, particularly in individuals with underlying vascular insufficiency and impaired healing capabilities associated with diabetes (Frykberg & Banks, 2015). Consequently, there is a growing need for innovative and adjunctive therapies that can enhance the healing process and improve outcomes for patients with DFUs in Pasco County and beyond.
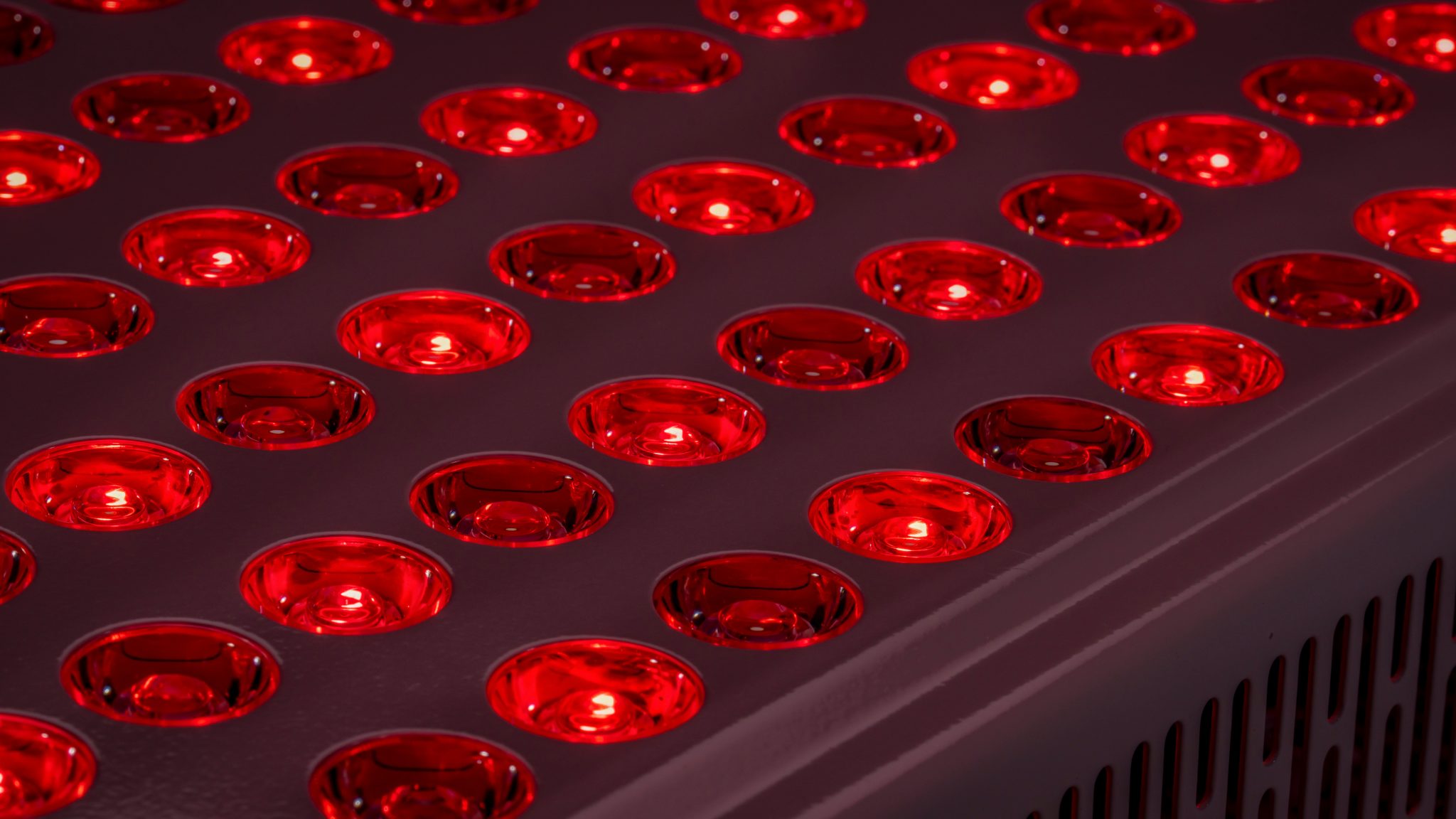
Red light therapy (RLT), also known as photobiomodulation (PBM), is a non-invasive therapeutic technique that utilizes low-level light at red and near-infrared wavelengths to stimulate cellular function and promote tissue repair (Hamblin & Anders, 2013). RLT has garnered increasing attention for its potential applications in various medical fields, including dermatology, pain management, and wound healing (Avci et al., 2013). This paper aims to explore the potential benefits of RLT as an adjunctive treatment for diabetic wounds, specifically considering its relevance and implications for individuals residing in Pasco County, Florida. By examining the mechanisms of action, reviewing existing clinical evidence, and considering the local context, this paper will assess the promise of RLT in addressing the challenges associated with DFU management in this community.
Mechanisms of Action of Red Light Therapy in Wound Healing
The therapeutic effects of RLT are mediated by the absorption of photons by specific chromophores within cells, primarily in the mitochondria (Karu, 1998). This absorption triggers a cascade of photochemical and photophysical events that ultimately lead to enhanced cellular function and tissue repair. Several key mechanisms contribute to the wound-healing benefits of RLT:
- Increased ATP Production: RLT stimulates the mitochondrial respiratory chain, leading to increased production of adenosine triphosphate (ATP), the primary energy currency of the cell. This enhanced energy availability supports energy-dependent cellular processes crucial for wound healing, such as cell proliferation, migration, and protein synthesis (Liebert et al., 2016).
- Modulation of Reactive Oxygen Species (ROS): While high levels of ROS can be detrimental, low levels play a crucial role in cell signaling and wound healing. RLT can help to modulate ROS levels, reducing oxidative stress in chronic wounds and promoting a more balanced cellular environment conducive to healing (Gupta et al., 2014).
- Enhanced Angiogenesis: The formation of new blood vessels (angiogenesis) is essential for delivering oxygen and nutrients to the wound site, supporting tissue regeneration. RLT has been shown to stimulate the release of growth factors, such as vascular endothelial growth factor (VEGF), which promotes angiogenesis and improves blood flow to the wound (Zupin et al., 2015).
- Stimulation of Collagen Synthesis: Collagen is a key structural protein in the extracellular matrix and plays a vital role in wound closure and tissue remodeling. RLT can stimulate fibroblasts, the cells responsible for collagen production, leading to increased synthesis of collagen and improved wound strength (Sorokina et al., 2018).
- Reduction of Inflammation: Chronic inflammation can impede wound healing in diabetic patients. RLT has demonstrated anti-inflammatory effects by modulating the release of pro-inflammatory cytokines and promoting the infiltration of anti-inflammatory cells (Houreld, 2008).
- Improved Cell Proliferation and Migration: RLT can stimulate the proliferation and migration of keratinocytes and fibroblasts, the key cell types involved in wound re-epithelialization and tissue repair (Russo et al., 2019).
These multifaceted mechanisms of action suggest that RLT can address several of the underlying factors that contribute to impaired wound healing in diabetic patients, making it a potentially valuable adjunctive therapy for DFUs in Pasco County.
Clinical Evidence for Red Light Therapy in Diabetic Wound Healing
A growing body of clinical research has investigated the efficacy of RLT in the treatment of diabetic wounds. While more large-scale, randomized controlled trials are needed, existing studies offer promising evidence for its benefits:
- Accelerated Wound Closure: Several studies have reported that RLT significantly accelerates the rate of wound closure in DFUs compared to standard care or placebo. For instance, a meta-analysis by Liu et al. (2017) concluded that low-level laser therapy (LLLT), which includes red and near-infrared light, can significantly improve the healing rate and reduce the size of diabetic ulcers.
- Reduced Pain: Diabetic neuropathy often accompanies DFUs, leading to significant pain and discomfort. Some studies have indicated that RLT can help to reduce pain levels in patients with diabetic wounds, potentially improving their quality of life and adherence to treatment (dos Santos et al., 2019).
- Improved Tissue Granulation and Epithelialization: RLT has been shown to promote the formation of healthy granulation tissue and accelerate the process of epithelialization, both crucial steps in wound healing (Ferreira et al., 2016).
- Reduced Risk of Infection: While not a primary antimicrobial therapy, some evidence suggests that RLT may have a modulating effect on the wound microenvironment, potentially reducing the risk of infection by improving tissue viability and immune response (Guffey et al., 2011).
These findings suggest that RLT holds significant potential as an adjunctive therapy to enhance the healing of diabetic wounds. While the specific protocols (wavelengths, energy densities, treatment durations) may vary across studies, the overall trend indicates a positive impact on wound healing outcomes.
Relevance and Implications for Pasco County, Florida
The potential benefits of RLT for diabetic wound healing have significant implications for the healthcare landscape in Pasco County, Florida. The county’s demographic profile, with a notable proportion of older adults, may contribute to a higher prevalence of diabetes and its associated complications, including DFUs (U.S. Census Bureau, 2020). Access to specialized wound care services and the economic burden of managing chronic wounds are important considerations in this region.
Integrating RLT into existing wound care protocols in Pasco County could offer several advantages:
- Improved Healing Outcomes: By accelerating wound closure and promoting tissue regeneration, RLT could lead to faster healing times and reduced complications for individuals with DFUs.
- Reduced Healthcare Costs: Faster healing and fewer complications could translate to lower healthcare costs associated with prolonged hospitalizations, wound care supplies, and potential amputations.
- Enhanced Quality of Life: Reduced pain, improved mobility, and faster return to daily activities could significantly enhance the quality of life for diabetic patients in Pasco County.
- Non-Invasive and Safe Therapy: RLT is a non-invasive and generally well-tolerated therapy with minimal reported side effects, making it a potentially attractive option for individuals with comorbidities or those who may not be suitable for more invasive treatments.
- Accessibility and Integration: RLT devices are becoming increasingly accessible and can potentially be integrated into various healthcare settings, including hospitals, clinics, and even home-based care under proper guidance. This could improve access to advanced wound care for patients in Pasco County, particularly those in rural or underserved areas.
However, the successful implementation of RLT for diabetic wound care in Pasco County would require:
- Awareness and Education: Healthcare professionals, including physicians, podiatrists, nurses, and wound care specialists in Pasco County, need to be educated about the evidence-based benefits and protocols for RLT in diabetic wound healing.
- Availability of Technology: Healthcare facilities and clinics in the region need to invest in appropriate RLT devices and ensure that trained personnel are available to administer the therapy.
- Standardized Protocols: The development and adoption of standardized treatment protocols for RLT in diabetic wound care would be essential to ensure consistent and effective outcomes.
- Further Research: While existing research is promising, further studies specifically examining the effectiveness of RLT in diverse patient populations and healthcare settings within Florida, including Pasco County, would be valuable. This could include investigating optimal treatment parameters, cost-effectiveness, and patient satisfaction.
Conclusion
Diabetic foot ulcers represent a significant health and economic challenge in Pasco County, Florida. Red light therapy has emerged as a promising adjunctive treatment for promoting wound healing through various cellular and molecular mechanisms. Existing clinical evidence suggests that RLT can accelerate wound closure, reduce pain, and improve tissue regeneration in diabetic wounds. While research specifically focused on Pasco County is lacking, the potential benefits of RLT align with the need for more effective and less invasive treatments for DFUs in this community. Integrating RLT into existing wound care protocols in Pasco County could lead to improved patient outcomes, reduced healthcare costs, and enhanced quality of life for individuals living with diabetes. At Caliper Wellness we offer RLT for varying disease processes including anxiety, depression, and so much more. Utilizing RLT for treatment of diabetic wounds opens the door for improved patient outcomes in our community which is our entire mission at Caliper Wellness. Schedule your appointment today with our Nurse Practitioner for an assessment to see if RLT is the right treatment for you.
References
Armstrong, D. G., Boulton, A. J. M., & Bus, S. A. (2017). Diabetic foot ulcers and their recurrence. The New England Journal of Medicine, 376(24), 2367-2375.
Avci, P., Gupta, A., Sadasivam, M., Vecchio, D., Pam, Z., Hamblin, M. R. (2013). Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Seminars in Cutaneous Medicine and Surgery, 32(1), 41-52.
Centers for Disease Control and Prevention. (n.d.). National Diabetes Statistics Report.
dos Santos, E. C. P., Nicolau, R. A., Stadler, J., Clark, C. P., & Hamblin, M. R. (2019). Photobiomodulation in the treatment of diabetic foot ulcers: a systematic review and meta-analysis. Lasers in Medical Science, 34(1), 53-63.
Ferreira, L. B., de Oliveira, D. A., Zângaro, R. A., & Soares, C. P. (2016). Low-level laser therapy in the treatment of chronic diabetic foot ulcers: a systematic review. International Wound Journal, 13(6), 1203-1211.
Florida Department of Health. (2024). Diabetes Surveillance Data.
Frykberg, R. G., & Banks, J. (2015). Challenges in the treatment of chronic wounds. Advances in Wound Care, 4(9), 560-569.
Guffey, J. S., Barrett, J. P., & Cummings, J. (2011). Low-level laser therapy as a treatment for chronic wounds: a review of the literature. Dermatologic Surgery, 37(12), 1617-1624.
Gupta, A., Dai, T., Hamblin, M. R. (2014). Effect of red/near-infrared light on reactive oxygen species in in vitro and in vivo systems. Journal of Photochemistry and Photobiology B: Biology, 137, 68-75.
Hamblin, M. R., & Anders, J. J. (2013). Mechanisms of low level light therapy. Proceedings of SPIE, 8615, 861501.
Houreld, N. N. (2008). Therapeutic efficacy of low-level laser therapy for chronic wounds. Lasers in Surgery and Medicine, 40(8), 511-519.
Karu, T. I. (1998). Molecular mechanisms of the therapeutic effect of low-intensity laser irradiation. Journal of Photochemistry and Photobiology B: Biology, 49(1), 1-17.
Liebert, A., Jagielska, J., Martens-Lobenhoffer, J., Bode-Böger, S. M., & Godlewski, G. (2016). Mitochondrial effects of photobiomodulation. Antioxidants & Redox Signaling, 24(1), 139-151.
Lipsky, B. A., Berendt, A. R., Cornia, P. B., Pile, J. C., Peters, E. J., Armstrong, D. G., … & Senneville, É. (2016). 2012 infectious diseases society of america clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clinical Infectious Diseases, 54(12), e132-e173.
Liu, X., Liu, T., Zhang, H., Li, J., & Zhang, Y. (2017). Efficacy of low-level laser therapy in the treatment of diabetic foot ulcers: a meta-analysis of randomized controlled trials. Lasers in Medical Science, 32(1), 21-29.
Russo, V., Trovato, L., Cannizzaro, G., Giustolisi, V., & Avci, P. (2019). Photobiomodulation in the management of diabetic foot ulcers: A narrative review. Journal of Clinical Medicine, 8(11), 1948.
Sorokina, E. G., Mamaev, A. N., & Mamaeva, E. V. (2018). Effect of low-intensity laser irradiation on collagen synthesis in fibroblasts in vitro. Biomedical Photonics, 7(3), 030501.
U.S. Census Bureau. (2020). QuickFacts: Pasco County, Florida.
Zupin, L., та ін. (2015). The effect of low-level laser therapy on angiogenesis in diabetic foot ulcers. Journal of Vascular Surgery, 62(3), 704-711.